Interdisciplinary Focus
“ Advancing clinical practice through united efforts in research, education, and cross-disciplinary collaboration. ”
— Dr. Winston R. Warren, EMT-P
Predicting Response to Naloxone in Patients with Respiratory Depression in the Prehospital Setting: A Retrospective Analysis Study.
ABSTRACT
Objectives
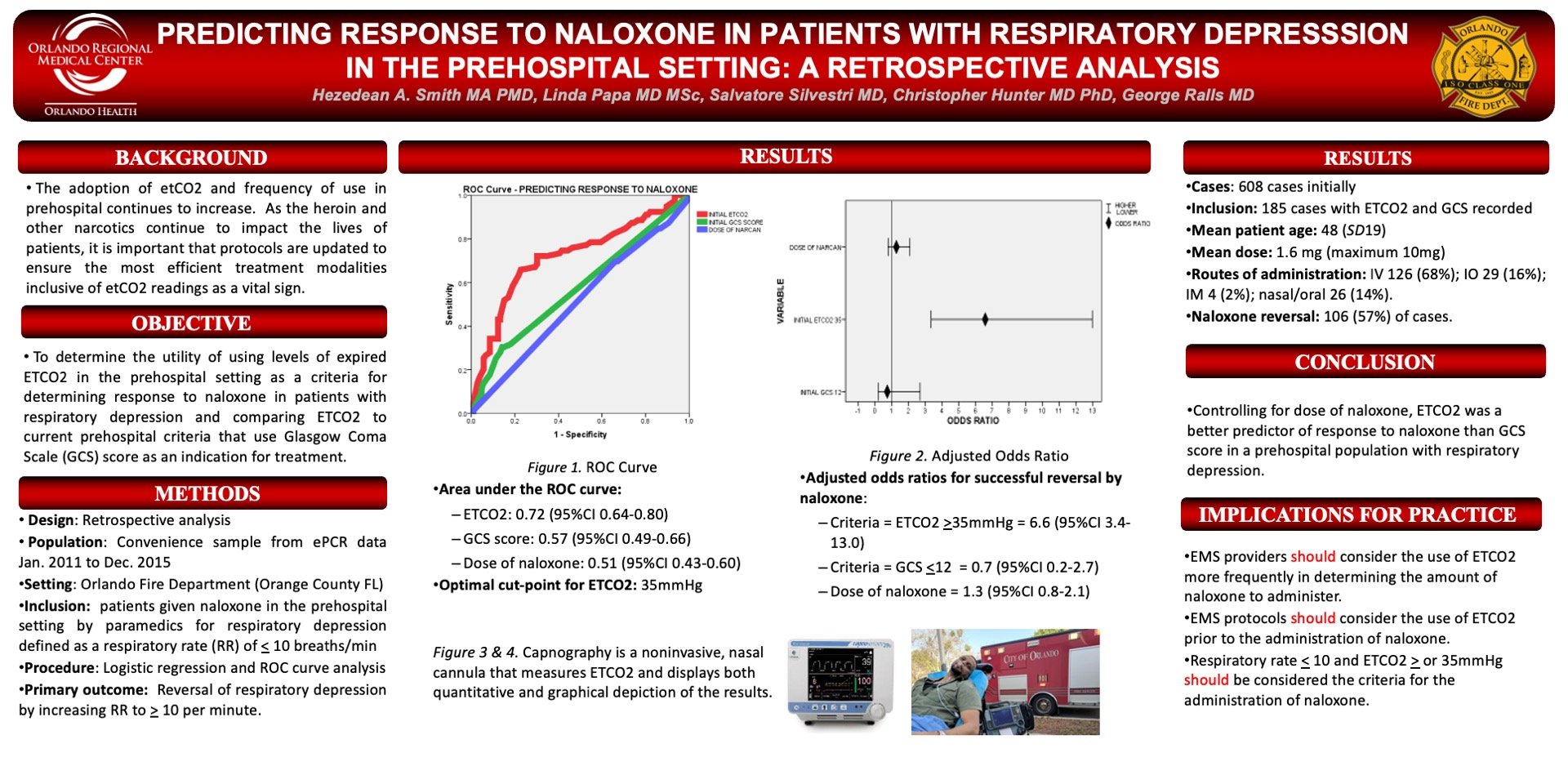
The objective of the study was to determine the utility of using levels of expired ETCO2 in the prehospital setting as a criterion for determining response to naloxone in subjects with respiratory depression, and comparing ETCO2 to current prehospital criteria that makes use of Glasgow Coma Scale (GCS) score as an indication for treatment.
Methods
A retrospective analysis of prospective prehospital EMS data collected from a single EMS agency in Florida was conducted. The case study comprised of all patients given naloxone in the prehospital setting by paramedics for respiratory depression – defined as a respiratory rate (RR) of less than or equal to 10 breaths per minute. The main outcome measure was the success of naloxone administration in reversing respiratory depression by increasing RR to greater than or equal to 10 breaths per minute. Data was adjusted to account for the dose of naloxone used as documented by the providers. Logistic regression and ROC curve analysis were conducted and expressed using 95%CI.
Results
Of the 608 cases initially identified, 185 cases had both ETCO2 and GCS recorded and as such, were included in the analysis. The mean patient age was 48 (SD = 19). The mean dose of naloxone administered was 1.6 mg (with a maximum of 10 mg) and the routes of administration included IV in 126 (68%), IO in 29 (16%), IM in 4 (2%), and nasal/oral in 26 (14%). Naloxone reversed respiratory depression in 106 (57%) of cases.
The area under the ROC curve for predicting response to naloxone using ETCO2 was 0.72, using the GCS score the result was 0.57 and using dose of naloxone the ROC curve was 0.51. Optimal cut-point for ETCO2 was determined to be 35mmHg. Adjusted odds ratios for successful reversal by naloxone by using criteria ETCO2 > 35mmHg was 6.6, for GCS < 12 it was 0.7, and for dose of naloxone the result was 1.3.
Conclusions
The researchers concluded that for controlling the dose of naloxone, ETCO2 was a better predictor of response to naloxone than GCS score in a prehospital population with respiratory depression.
KEYWORDS
Naloxone; Narcan; end-tidal carbon dioxide; overdose; respiratory depression
Researchers:
INTRODUCTION
The use of naloxone (narcan) in suspected cases of opiate patients continues to increase in the prehospital care provided by emergency medical services (EMS) providers. The frequency of administration of narcan to patients has been found to vary depending on race and age (Irwin et al., 2017). In Orange County, Florida, the number of suspected heroin-related overdoses has continued to rise, however deaths resulting from heroin-related overdoses have declined by 56 percent in 2017 (Medel, 2017). In major cities across the United States, the heroin crisis has brought Fire-based EMS agencies and Law Enforcement agencies together to examine methods of improving care and mitigating the crisis (Irwin et al., 2017).
The Orlando Fire Department initiated fire-based EMS transport in 2011 with a fleet of 11 advanced life support (ALS) transport units, 18 ALS engines, 7 ALS ladder trucks, and 1 ALS Heavy Rescue unit. The ALS units are staffed with a minimum of at least one ALS provider and one basic life support provider. The Orlando Fire Department transports over 20,000 EMS calls each year.
As the frequency of administration, and cost of naloxone continues to increase, it is important from a quality improvement perspective to appraise the use of naloxone, protocols, and its implications on patient outcome. The EMS Division uses a cloud-based solution to maintain electronic ‘patient care records’ of every patient encounter collected via computer tablets.
The use of capnography, assessment of Glasgow Coma Scale (GCS) scores and respiratory rates were essential considerations for the study. The problem is, since 2011, the local EMS system has not evaluated the use of naloxone through a quantitative approach. The protocols guiding the use of naloxone had not been re-examined in over five years. The existing practice parameters were released by the Orange County (FL) Office of Medical Directors in 2012, and are now under revision. The current practice protocol used by the local agency requires the following criteria to be met prior to the administration of naloxone: significantly altered mental status, a GCS <¬ 12, and respiratory rate < 10 breaths per minute and, as such were the parameters used as the benchmark for inclusion or exclusion.
The purpose of the study was to determine the utility of using levels of expired ETCO2 in the prehospital setting. It was used as a criterion for determining response to naloxone in patients with respiratory depression and comparing end-tidal carbon dioxide (ETCO2) to current prehospital criteria that uses Glasgow Coma Scale (GCS) score as an indication for treatment. The researchers recognized that naloxone should be used to ensure patients are breathing effectively after its administration. Oftentimes, medical providers report the respiratory rates of patients inaccurately (Manifold, Davids, Villers, & Wampler, 2013).
The use of capnography, which is more reliable, has become the standard of care in airway management of the non-intubated and oftentimes obtunded patients in the prehospital field (Martin, Silvestri, Papa, Ralls, & Krauss, 2007; Manifold, Davids, Villers, & Wampler, 2013). The concern for the increased cost associated with the frequency of naloxone use was also an underlying concern for management. In 2016, depending on the formulation, the cost of naloxone used as indicated by major vendors has increased from a range of 129% to 500% since 2012 (Gupta, Shah, & Ross, 2016). While it was expected that the use of ETCO2, which is a measurement of ventilation, is a much better predictor of response to naloxone than GCS, the analysis of the data was important.
The objectives of the study were to identify specific methods for improving the delivery of patient care in the prehospital management of patients suspected of a narcotic overdose and identifying opportunities for cost containment based on quantifiable measures. End-tidal carbon dioxide (ETCO2) is reflective of a person’s metabolism and respiratory efficiency (Nagurka et al., 2014).
METHODS
The study was a retrospective correlational design that included EMS data collected from the single fire-based EMS agency related to the administration of naloxone in Orange County, Florida. The Orlando Regional Medical Center (ORMC) Institutional Review Board (IRB) determined the study was exempt from IRB review in accordance to federal regulations. The study period was between January 1, 2011 and December 31, 2015. The de-identified data were obtained electronically from the electronic ‘patient care records’ database as a Microsoft Excel file. The researcher examined the data for any entry errors. Validity and reliability of the data were addressed via the confirmation of information previously submitted as the documentation of patient care activities provided by licensed EMS providers (paramedics) within the system. Documentation errors in the sample were controlled by excluding missing, erroneous, or obviously incorrect data elements.
For GCS scores reported as 0, such cases were excluded from the analysis (Bledsoe et al., 2015). The lowest GCS score included in the study was three (3) and the highest was fifteen (15). Respiratory rates ranging from zero (0) to sixty (60) in adult patients were included in the sample.
The study was determined exempt by the Orlando Health – Orlando Regional Medical Center’s Institutional Review Board (Orlando, Florida, USA). The sample population included only patients with respiratory rates less than or equal to 10 breaths per minute, who were given naloxone in the prehospital setting by paramedics. All ranges for end-tidal carbon dioxide were included with the exception of three-digit numbers.
ANALYSIS
The independent variables in the study were the initial respiratory rate, GCS, and end-tidal carbon dioxide readings. These independent variables are used by prehospital providers to determine the dose of naloxone to be administered to obtain the final respiratory rate and an improvement in mental status. The independent variables were also reported on a nominal scale.
The dependent variable is the final respiratory rate of the patient. The change in the respiratory rate is dependent on the findings of the above-mentioned independent variables. If positive respiratory outcomes are observed by the EMS provider, the changes would be determined to be associated with the administration of naloxone regardless of the dose given. The dependent variable (final respiratory rate) was reported on a nominal level.
Threats to internal validity were minimized whereas, the total GCS score, end-tidal carbon dioxide level, and respiratory rate were the bases for the analysis. It is understood that the computation of the total GCS is very subjective and often inaccurately reported (Bledsoe et al., 2015). An initial number of cases (N = 608) was identified from the database. Cases inclusive of both ETCO2 and GCS were extrapolated (n = 185). The age of the patients was reported in the ePCR (n = 185, Mean = 48, SD = 19). The dose of naloxone was also documented in the ePCR by the paramedic completing the report with a maximum dose of 10 mg (Mean = 1.6 mg).
The route of administration of naloxone to the participating patients varied between: intravenous 126 (68%); intraosseous 29 (16%); intramuscular 4 (2%); and nasal/oral 26 (14%). The initial ETCO2 values were re-coded to establish a further understanding of the frequencies based on values below and above normal. The assessment of ETCO2 by EMS providers is by placing the device appropriately in the patient’s nose or by obtaining it through the use of bag-mask ventilation. Both techniques are appropriate based on the circumstance. The ETCO2 readings in the non-intubated patients were obtained using side-stream capture and analysis.
The main outcome measure was the success of naloxone administration in reversing the effects of respiratory depression. The basis of this outcome was a respiratory rate greater than or equal to 10 breaths per minute. The data was adjusted to account for the doses of naloxone administered in the sample. Logistic regression and receiver operating characteristic (ROC) curve analysis were done and reported with a 95% CI.
RESULTS
The Receiver Operating Characteristic (ROC) curve was used to evaluate the sensitivity and specificity of the efficacy of naloxone based on the dose administered and the outcome variable, which was the respiratory rate. The test variable was the respiratory rate, while the state variable equaled the outcome (respiratory rate change to > 10).
In 57% (106) of the extrapolated cases, naloxone was effective in reversing the clinical symptoms of the patients.
The following results are depicted in Figure 1: ETCO2 – 0.72 (95% CI 0.64 – 0.80); GCS score – 0.57 (95% CI 0.49 – 0.66); and dose of naloxone – 0.51 (95% CI 0.43 – 0.60)
A linear regression was used to conduct an analysis of the data. The optimal cut-point set for ETCO2 was 35 mmHg. The odds ratio (OR) was used to compare the relative odds of the occurrence of the outcome of interest, which was a ‘positive’ change in respiratory rate based on naloxone administration (see Figure 2). The only significant predictor of outcome was ETCO2 at > 35mmHg (6.6, 95% CI 3.4 – 13.0). The adjusted odds ratios were as follows, for GCS < 12 (0.7, 95% CI 0.2 – 2.7) and dose of naloxone (1.3, 95% CI 0.8 – 2.1).
DISCUSSION
The use of ETCO2 continues to expand in the prehospital care of patients across a broad spectrum. Prehospital providers should consider using ETCO2 as an additional assessment and a treatment guide. The use of ETCO2 when administering naloxone, can provide information regarding the effectiveness of naloxone based on the quantitative and graphical depiction of changes in ETCO2.
In many cases, during the attempted resuscitation of cardiac arrest patients, prehospital providers often administer naloxone in cases where there is a suspicion or lack thereof, of a narcotic overdose. Prehospital providers may also have to consider higher doses of naloxone due to the suspected nature of the overdose that may include combinations of opiates. The use of ETCO2 can also provide information to support those treatment decisions, however, the analysis did not focus on that subset of the population in this study. In some cases, the researchers noted that a high dose of naloxone was administered. The higher dose may have been attributed to situations involving a combination of narcotics or other unknown cause.
The researchers were hopeful of a larger sample size, however based on the compliance and other unknown circumstances, the cases included were only specific to those that had documented ETCO2 and GCS scores. A larger, more geographically dispersed patient population may have yielded similar or different results. The ROC curve analysis appeared to have sufficient strength as a statistical test. In cases where naloxone failed to reverse the respiratory depression, it was suspected that the patient’s lack of response might have been a result of other conditions versus a narcotic overdose.
CONCLUSION
Based on the findings of this study, EMS personnel should consider the use of ETCO2 in determining the amount of naloxone to administer. It is also recommended that practice parameters should be updated to reflect the requirement of ETCO2 assessment prior to the administration of naloxone and only administer naloxone in patients with a respiratory rate less than or equal to 10 and ETCO2 greater than or equal to 35 mmHg.
Controlling for the dose of naloxone to be administered, ETCO2 was a better predictor of response to naloxone than GCS score in the prehospital sample patients with respiratory depression. GCS scores are not only unreliable but also very subjective to inconsistencies with interrater reliability (Baker M, 2008; Bledsoe et al., 2015). The role of prehospital ETCO2 in narcotic overdoses should be further studied. ETCO2 must continue to be a part of EMS protocols.
Medical directors should consider requiring the application of ETCO2 prior to the administration of naloxone and during treatment and monitoring of such patients. As the opiate epidemic continues to claim the lives of citizens, it is important that EMS systems apply the findings of research in changing medical protocols for treatment. The ultimate aim is to improve patient care through the application and extensive use of side-stream or in-line/mainstream capnography.
The implications for educators and clinicians are for the continuous use of ETCO2, if available in an EMS system. Educators should incorporate ETCO2 in simulation education in an effort to improve cognitive competencies of learners. Future researchers may examine the administration of naloxone solely based on the reported ETCO2. Patients often, will suffer varied physiologic responses and often have a combination of drugs in their system, thus this study may have limited value in prediction potential. However, the continuous use and access to ETCO2 equipment should also contribute to improvement in treatment and subsequent patient outcomes.
AUTHORS
Assistant Chief Hezedean A. Smith served as the EMS Chief at the Orlando Fire Department and has been in EMS for over 30 years. He is currently the Assistant Chief assigned to Information and Technology. He is currently pursuing his Doctor of Management in Organizational Leadership at the University of Phoenix, School of Advanced Studies. He is a credentialed Chief Fire Officer, Certified Ambulance Compliance Officer, Executive Fire & Emergency Services Officer, Certified Public Manager and a Certified Healthcare Simulation Educator.
Salvatore Silvestri, MD, is the past Associate Medical Director at the Orange County Emergency Medical Services (Orlando, Florida) who passed away in February 2017. Dr. Silvestri mentored many physicians and EMS providers throughout his career. After arrival in Orange County, FL, he contributed significantly to the primary researcher’s goal of publishing research in support of capnography.
Linda Papa, MD, is the Director of Clinical Research at Orlando Health. Dr. Papa provided guidance and support for the quantitative analysis of the data discussed in the article.
Christopher Hunter, MD, PhD, FACEP, FAEMS, serves as an Associate Medical Director for the Orange County (Florida) Office of Medical Directors. He is the Assistant Program Director, Orlando Health Emergency Medicine Residency.
George Ralls, MD, FACEP, is currently the Director of Health and Public Safety at Orange County Government and also supports all aspects of the Office of Medical Directors (Orange County, Florida).
REFERENCES
Irwin, A., Jozaghi, E., Weir, B. W., Allen, S. T., Lindsay, A., & Sherman, S. G. (2017). Mitigating the heroin crisis in Baltimore, MD, USA: a cost-benefit analysis of a hypothetical supervised injection facility. Harm Reduction Journal; London, 14. doi:10.1186/s12954-017-0153-2
Baker M. (2008). Reviewing the application of the Glasgow Coma Scale: does it have interrater reliability? British Journal of Neuroscience Nursing, 4(7), 342–347.
Bledsoe, B. E., et al. (2015). Glasgow Coma Scale Scoring is Often Inaccurate. Prehospital and Disaster Medicine, 30(1), 46–53. doi:10.1017/S1049023X14001289
Lindstrom, H. A., et al. (2015). Prehospital Naloxone Administration as a Public Health Surveillance Tool: A Retrospective Validation Study. Prehospital and Disaster Medicine, 30(4), 385–389. doi:10.1017/S1049023X15004793
Nagurka, R., et al. (2014). Utility of Initial Prehospital End-tidal Carbon Dioxide Measurements to Predict Poor Outcomes in Adult Asthmatic Patients. Prehospital Emergency Care, 18(2), 180–184. doi:10.3109/10903127.2013.851306
Martin, D. L., et al. (2007). Capnography as a Determinant of Ventilatory Status for Out-of-Hospital Obtunded Patients. Annals of Emergency Medicine, 50(3), S92. doi:10.1016/j.annemergmed.2007.06.278
Medel, S. (2017). Orange County begins 2017 with marked rise in heroin overdoses - Orlando Sentinel.
Gupta, R., Shah, N. D., & Ross, J. S. (2016). The Rising Price of Naloxone -- Risks to Efforts to Stem Overdose Deaths. The New England Journal of Medicine, 375(23), 2213–2215. doi:10.1056/NEJMp1609578
Manifold, C. A., et al. (2013). Capnography for the Nonintubated Patient in the Emergency Setting. The Journal of Emergency Medicine, 45(4), 626–632. doi:10.1016/j.jemermed.2013.05.012